Introduction
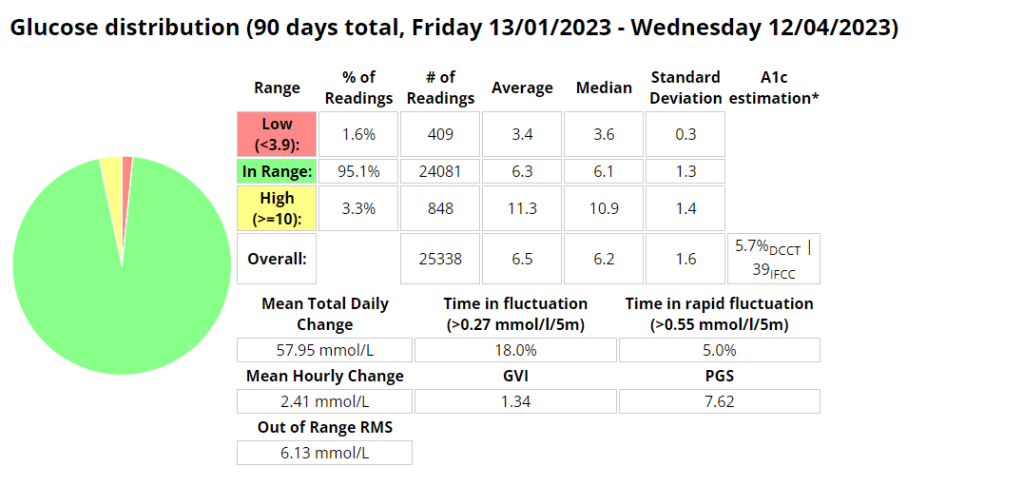
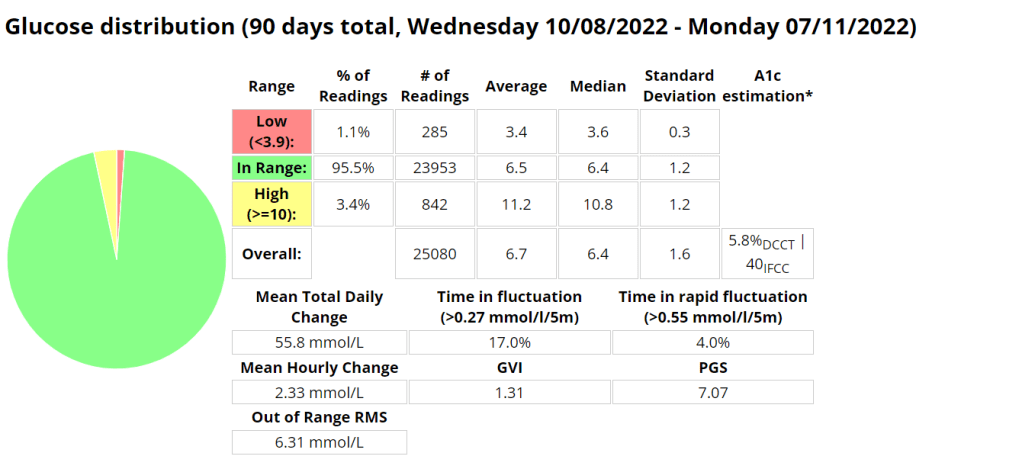
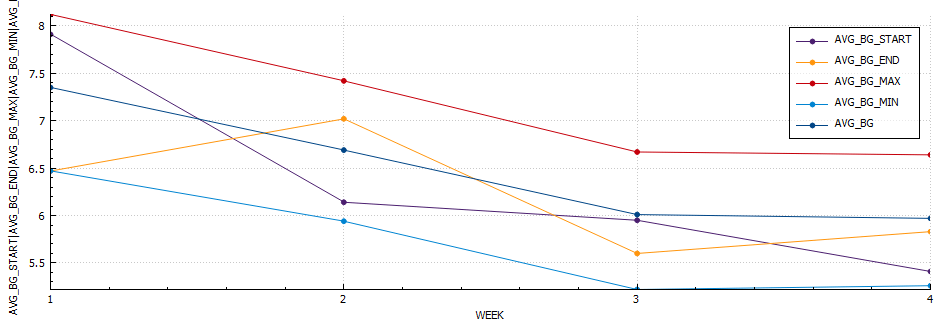
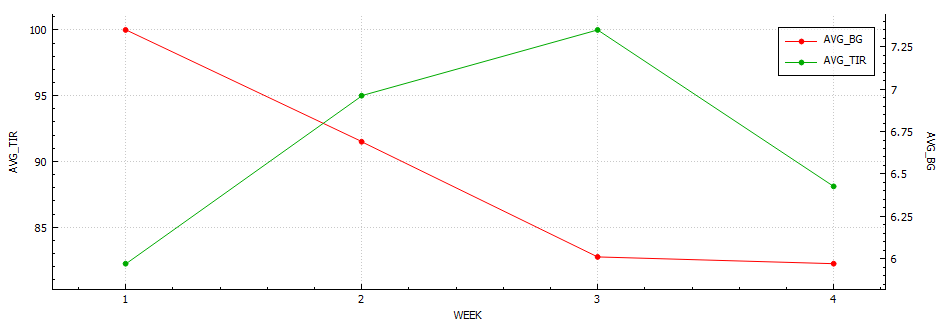
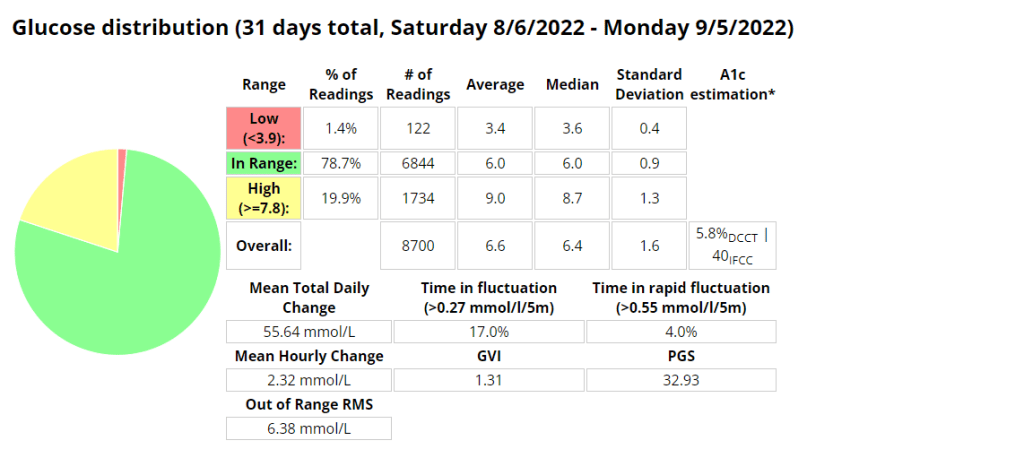
For individuals living with diabetes, maintaining stable blood glucose levels is a critical aspect of managing their condition effectively. Traditionally, glycated hemoglobin (HbA1c) has been the primary metric for evaluating long-term glucose control. However, it provides only a snapshot of average glucose levels over several months. To gain deeper insights into daily glycemic patterns and fluctuations, healthcare professionals and patients are turning to a more comprehensive and dynamic metric called “Time in Tighter Range” (TITR).
What is Time in Tighter Range (TITR)?
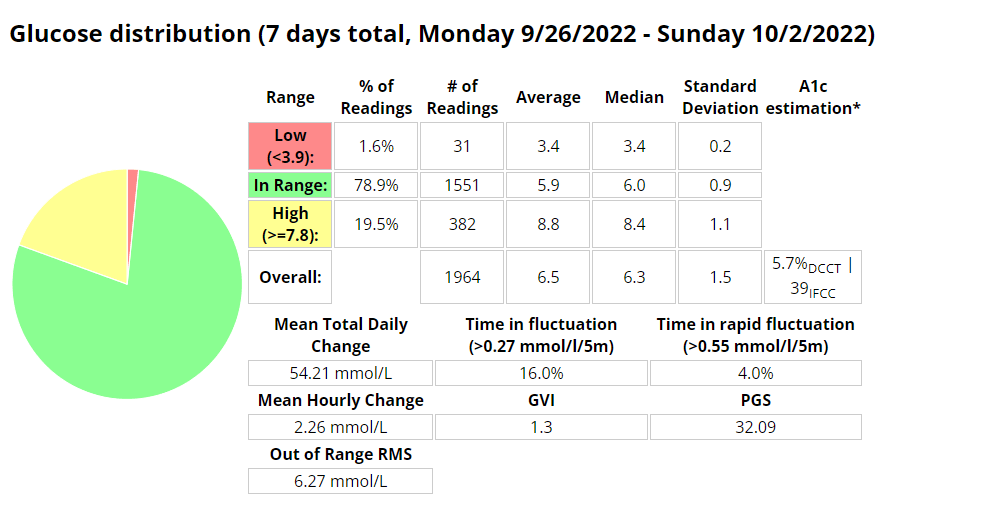
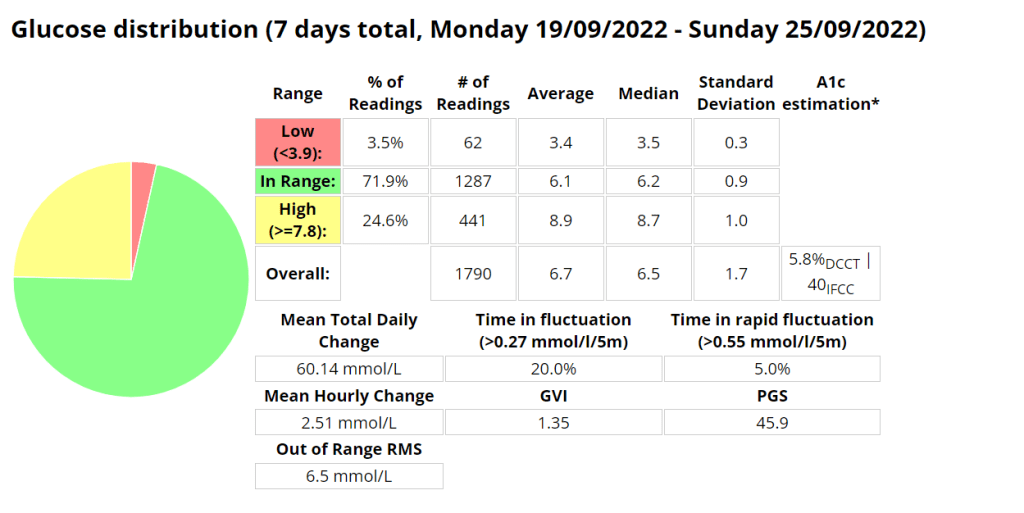
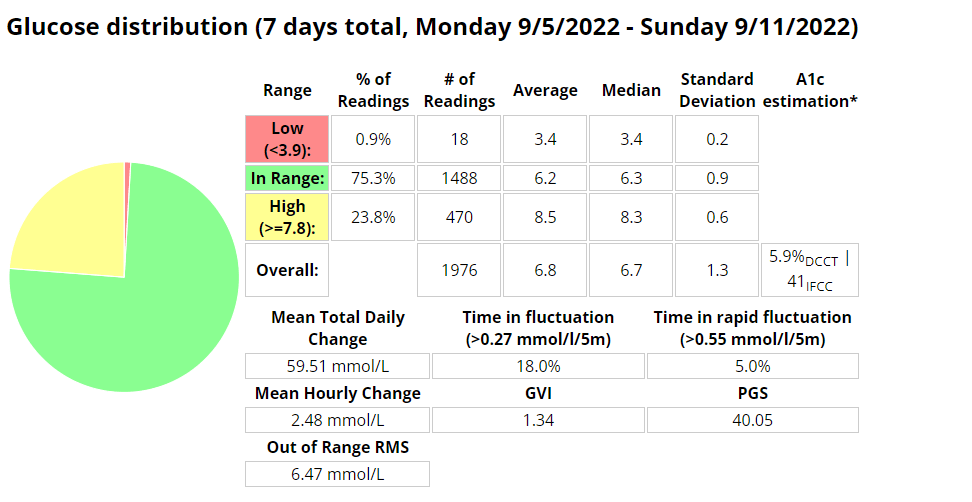
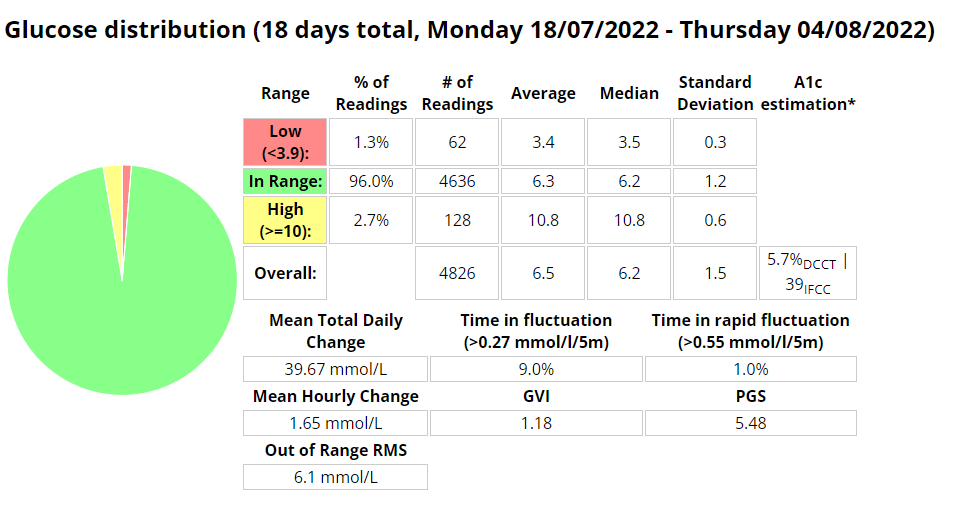
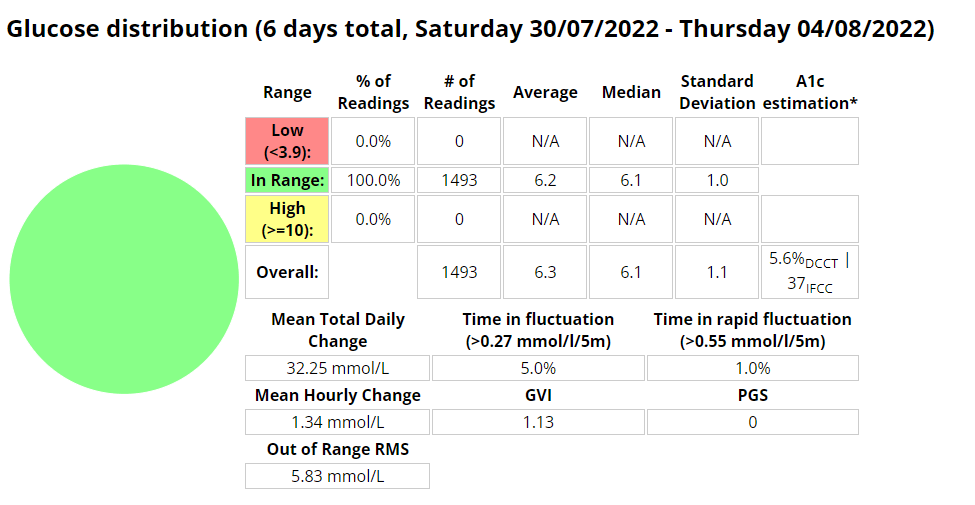
Time in Tighter Range (TITR) is a metric that quantifies the percentage of time blood glucose levels remain within a specific target range. The target range is often defined as the optimal window where glucose levels are considered both safe and effective in reducing the risk of diabetes-related complications. Commonly, the TITR target range is set between 70-140 mg/dL (3.9-7.8 mmol/L), but it can be tailored to an individual’s needs based on age, health status, and treatment goals.
Why TIR Matters in Diabetes Management
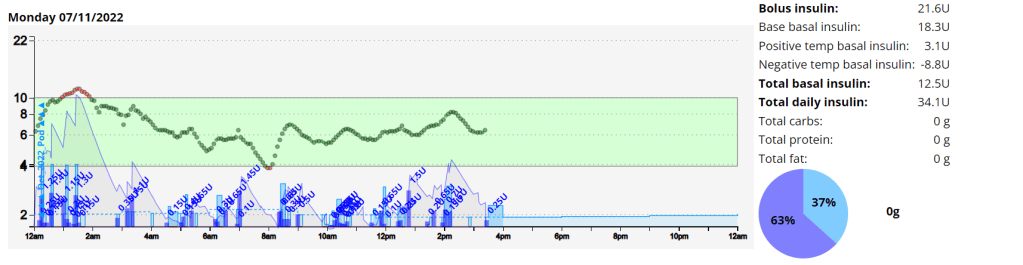
- Real-Time Assessment: Unlike HbA1c, which provides a retrospective average, TIR offers real-time data, empowering patients and healthcare professionals to make immediate adjustments to diabetes management strategies.
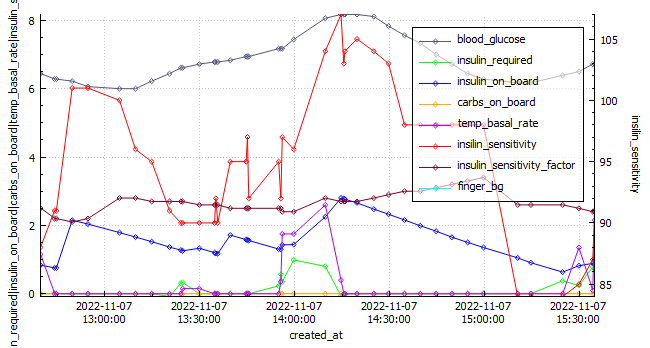
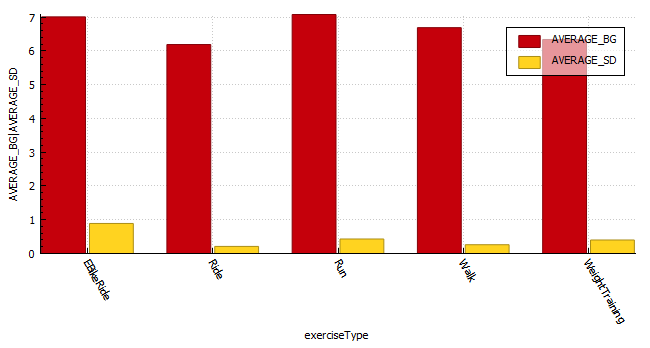
- Insights into Glucose Patterns: TITR helps reveal patterns and trends in glucose control, identifying potential trouble spots and offering opportunities for targeted interventions.
- Reduction of Hypoglycemia and Hyperglycemia: Maintaining TIR within the target range can reduce both hypoglycemic episodes (dangerously low blood glucose levels) and hyperglycemia (elevated blood glucose levels), enhancing overall quality of life and mitigating diabetes-related complications.
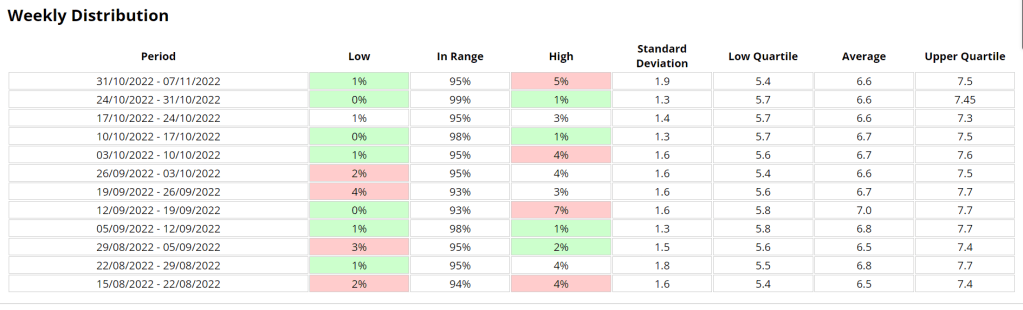
Tracking and Monitoring with TITR
Using TIR involves continuous glucose monitoring (CGM) or frequent blood glucose measurements. The data is then analyzed to determine the percentage of time spent within the target range. Several approaches can be used to track TIR:
- CGM Devices: Advanced CGM devices automatically calculate and display TIR data, offering users real-time feedback on their glucose control.
- Data Logs: Patients and healthcare professionals can manually record blood glucose readings and calculate TIR using spreadsheets or dedicated apps.
TITR in Real-Life Scenarios
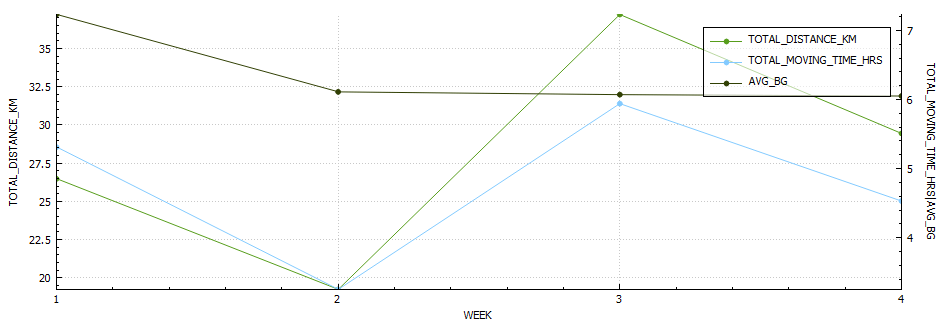
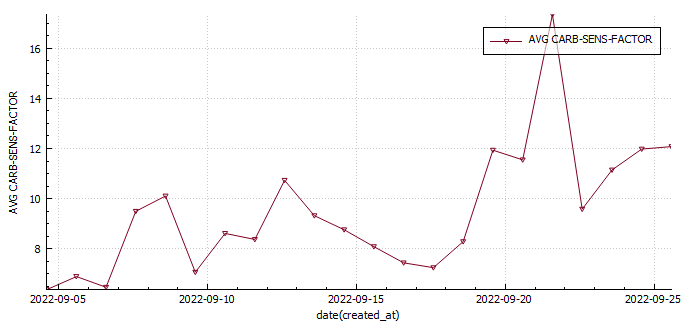
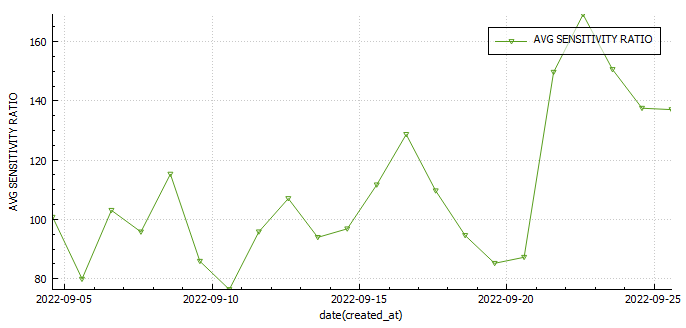
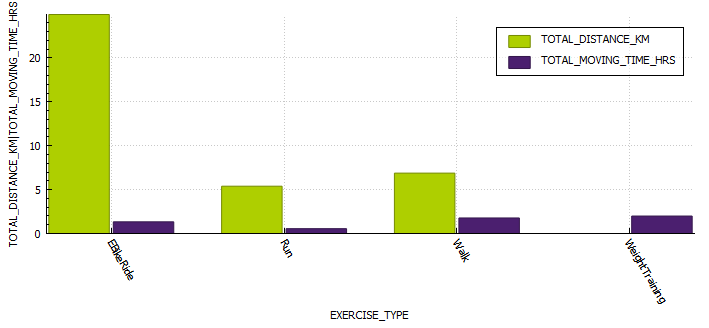
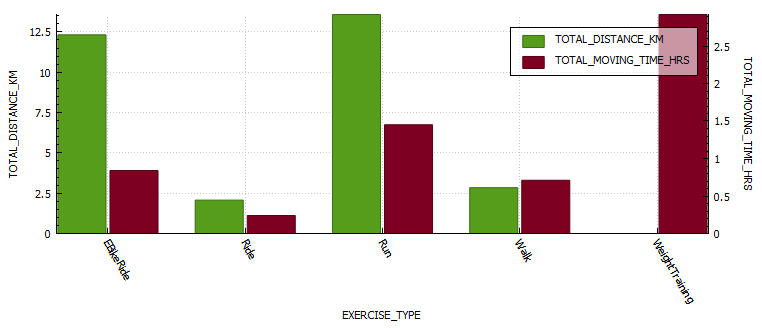
- Personalized Diabetes Management: TITR allows for a tailored approach to diabetes management. It helps healthcare professionals customize treatment plans and make timely adjustments to insulin dosing, diet, and exercise regimens.
- Pregnancy and Diabetes: During pregnancy, TITR is critical for expectant mothers with diabetes, as tight glucose control is vital for the health of both the mother and the baby.
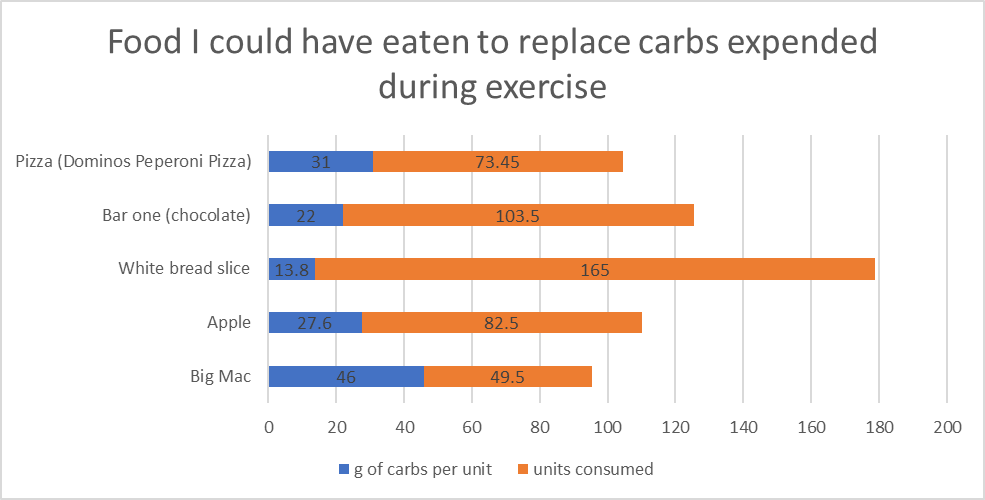
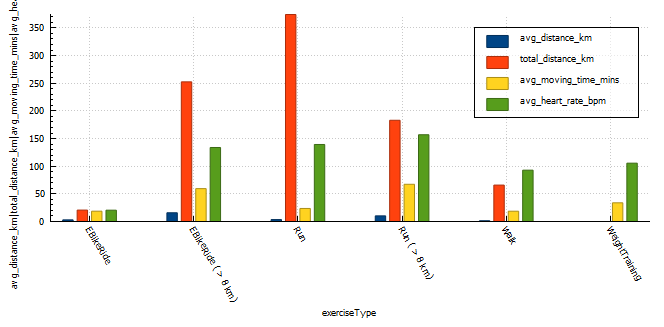
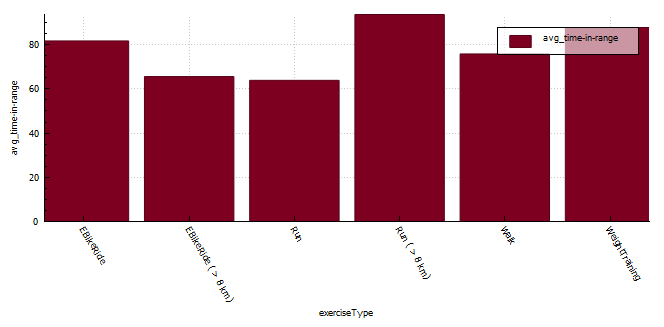
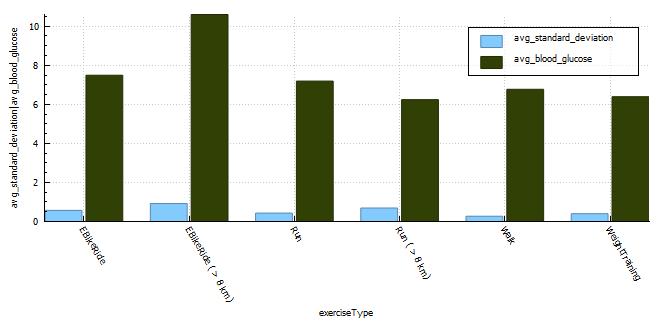
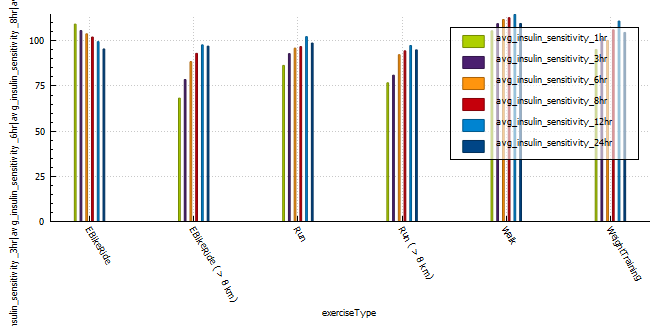
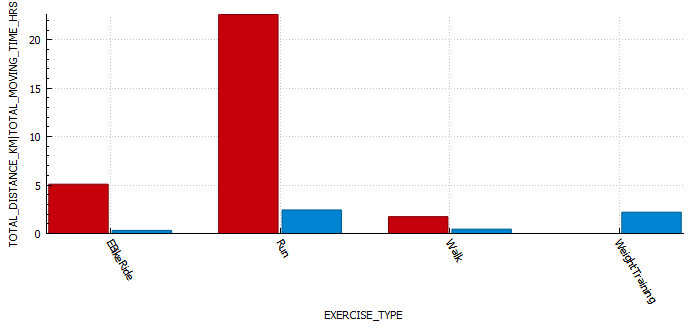
- Sports and Physical Activity: For athletes with diabetes, TITR provides insights into glucose fluctuations during physical activity, helping them optimize performance and avoid glucose-related issues during exercise.
Conclusion
Time in Tighter Range (TITR) is a valuable and dynamic metric that goes beyond traditional HbA1c measurements, providing real-time insights into daily glycemic patterns. With its ability to track fluctuations and trends within the target range, TITR empowers individuals and healthcare professionals to take proactive steps towards better diabetes management. By striving for optimal TITR, patients can enhance their quality of life, reduce the risk of complications, and achieve greater control over their diabetes. As TITR continues to gain prominence in diabetes care, it offers new possibilities for personalized and effective diabetes management strategies.